The image of a young woman clutching her arm, the sight of fresh cuts etched across her skin, is a stark reminder of the silent pain that can be hidden behind a seemingly normal facade. This is the reality of self-harm, a deeply troubling behavior that affects countless individuals across all demographics. As healthcare providers, we must acknowledge the human cost of this crisis and actively seek ways to intervene, support, and heal. The development of a comprehensive nursing care plan for individuals at risk for self-mutilation is critical in their journey towards recovery and well-being.
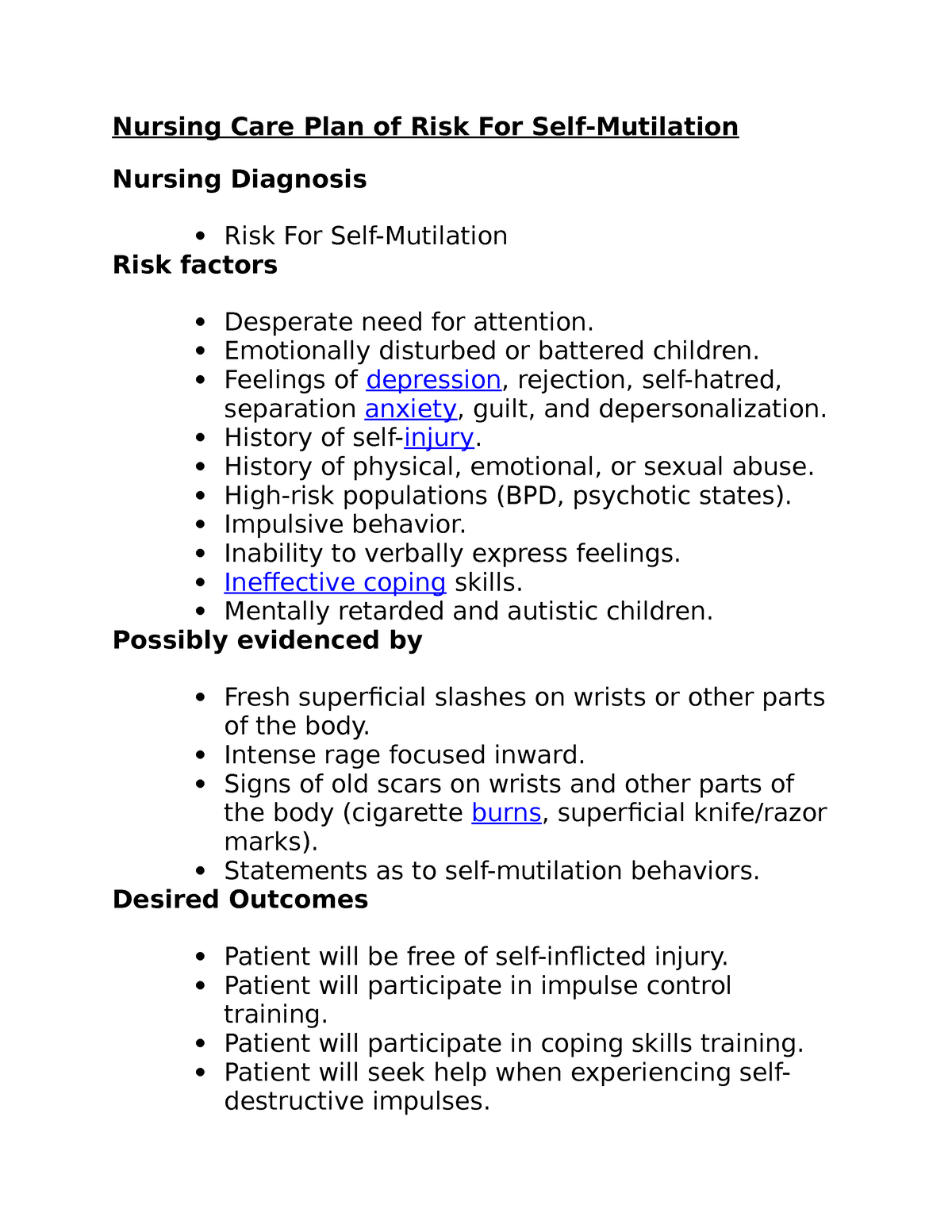
Image: www.studocu.com
This article will delve into the complexities of self-mutilation, exploring its underlying causes, identifying crucial risk factors, and outlining a comprehensive nursing care plan. Through a detailed exploration of the subject, we aim to empower nurses with the knowledge and tools needed to provide empathetic and effective care to individuals struggling with this challenging issue.
Understanding Self-Mutilation: A Deeper Look
Self-mutilation, also known as non-suicidal self-injury (NSSI), is a complex and often misunderstood behavior. It involves intentionally causing harm to oneself without the intent to end one’s life. While the outward actions may seem extreme, the underlying causes are often rooted in profound emotional distress, a struggle to cope with overwhelming feelings, and a desperate attempt to alleviate mental agony.
The history of self-mutilation dates back centuries, with evidence surfacing in various cultures and societies. Ancient civilizations, including the Greeks and Romans, documented practices of self-inflicted pain as rituals, expressions of grief, or ways to appease deities. In modern times, self-mutilation has gained increased attention within the medical and psychological fields, leading to a greater understanding of its multifaceted nature and the need for specialized care.
Factors Contributing to Self-Mutilation
There is no single cause for self-mutilation. Rather, it is a complex interplay of biological, psychological, and social factors. Understanding these contributing elements is essential for developing effective interventions.
Biological Factors:
Some research suggests that individuals who self-injure may have differences in their brain chemistry or neurobiology, specifically in areas associated with pain regulation, impulsivity, and emotional processing. Certain neurochemicals, such as serotonin and norepinephrine, are believed to play a role in mood and impulsivity, and imbalances in these chemicals may contribute to self-harm behaviors.

Image: www.scribd.com
Psychological Factors:
The psychological factors underlying self-mutilation are often deeply personal and varied. Some individuals might engage in self-harm as a way to cope with overwhelming emotions, such as intense anger, sadness, anxiety, or feelings of emptiness and dissociation. They may be struggling with underlying mental health conditions such as depression, anxiety disorders, post-traumatic stress disorder (PTSD), or borderline personality disorder. Self-harm can also be a way to release pent-up tension, express inner turmoil, or seek a sense of control amidst chaotic experiences.
Social Factors:
Social factors, such as family dynamics, peer pressure, and cultural influences, can all contribute to the development of self-harm behaviors. Individuals who have experienced trauma, abuse, neglect, or bullying may be at a higher risk for self-mutilation. Negative social interactions, lack of support systems, and feelings of isolation can further exacerbate underlying psychological distress.
Developing a Comprehensive Nursing Care Plan
A well-structured nursing care plan for individuals at risk for self-mutilation is critical in their journey toward recovery. The plan should be tailored to the individual’s specific needs, taking into account their medical history, psychological profile, and social circumstances. Here’s a detailed guide to creating a comprehensive plan:
Assessment
The first step is to conduct a thorough assessment of the individual’s risk factors, current emotional state, and potential triggering situations. This involves gathering information through a structured interview, reviewing medical records and collateral information, and utilizing validated assessment tools. Important aspects of the assessment include:
- Identifying the frequency, severity, and methods of self-harm
- Assessing the individual’s overall mental health, including signs of depression, anxiety, or other mental health disorders
- Exploring the individual’s coping mechanisms and support system
- Identifying any underlying trauma, abuse, or stressors
- Assessing the individual’s risk of suicide or other self-harm behaviors
Goals and Interventions
Based on the assessment findings, clear and realistic goals should be established in collaboration with the individual, their family, and any other relevant healthcare professionals. The goals may focus on:
- Reducing the frequency and severity of self-harm behaviors
- Promoting healthy coping mechanisms
- Improving emotional regulation and stress management skills
- Addressing underlying mental health conditions
- Building a supportive network and fostering connection
Interventions should be individualized and may include:
- Therapeutic interventions: Psychotherapy, such as cognitive behavioral therapy (CBT), dialectical behavior therapy (DBT), or psychodynamic therapy, can help individuals identify and challenge negative thought patterns, develop healthier coping strategies, and manage intense emotions.
- Medication management: Antidepressants, anti-anxiety medications, or mood stabilizers may be prescribed to address underlying mental health conditions.
- Safety planning: Collaborating with the individual to develop a personalized safety plan that outlines strategies for managing urges to self-harm, such as identifying triggers, seeking support from trusted individuals, engaging in calming activities, and creating a safe environment.
- Self-harm management techniques: Teaching the individual different techniques to manage urges and cope with distress, such as grounding exercises, deep breathing, mindfulness practices, journaling, or engaging in creative outlets.
- Support groups: Connecting individuals with peer support groups, such as those provided by organizations like the National Alliance on Mental Illness (NAMI) or the Jed Foundation, can foster a sense of community, decrease isolation, and provide a safe space for sharing experiences and receiving empathy.
Evaluation and Follow-Up
Regular evaluation and follow-up are essential to monitor the individual’s progress and adjust the nursing care plan as needed. This may involve:
- Monitoring the individual’s emotional state, self-harm behaviors, and overall well-being.
- Assessing the effectiveness of interventions and making necessary adjustments.
- Providing ongoing support and guidance to the individual and their family.
- Establishing a plan for long-term management, including ongoing therapy, medication, and support services.
Latest Trends in Self-Mutilation Care
The field of mental health is constantly evolving, with new research and innovative approaches emerging to address the complexities of self-harm. Some of the latest trends in self-mutilation care include:
- Increased emphasis on trauma-informed care: Acknowledging the prevalence of trauma and its impact on self-harm behaviors, many healthcare providers are incorporating trauma-informed principles into their practice, creating a safe and supportive environment for individuals who have experienced trauma.
- Focus on mindfulness and acceptance-based therapies: Mindfulness-based therapies, such as Dialectical Behavior Therapy (DBT) and Acceptance and Commitment Therapy (ACT), are gaining popularity for their emphasis on accepting difficult feelings and developing skills for managing emotional distress.
- Integration of technology-based interventions: Mobile apps and online platforms designed to support individuals with self-harm behaviors are becoming increasingly common. These tools provide access to resources, tracking of self-harm episodes, and on-demand coping strategies.
Tips for Providing Effective Care
Nurses play a vital role in supporting individuals at risk for self-mutilation. Here are some key tips for providing effective care:
- Promote a non-judgmental and supportive environment. Avoid labeling or shaming the individual for their self-harm behaviors, and instead focus on understanding the underlying distress and providing support.
- Active listening and empathy are essential. Allow the individual to share their experiences and feelings without interruption or judgment. Empathy involves understanding the individual’s perspective and acknowledging their emotions without minimizing their suffering.
- Educate yourself about self-harm. Gaining knowledge about the causes, risk factors, and effective interventions for self-harm can help you provide more informed and compassionate care.
- Collaborate with other healthcare professionals. Work closely with psychiatrists, therapists, and other mental health professionals to ensure the individual receives comprehensive care.
- Encourage the individual to seek professional help. Support them in finding a therapist or other mental health professional who can provide specialized interventions.
- Advocate for the individual’s needs. Advocate for appropriate treatment, resources, and support services to help the individual on their path to recovery.
FAQs about Self-Mutilation
What are some common signs and symptoms of self-mutilation?
Signs and symptoms vary widely, and individuals may not always display all of them. Some common signs include:
- Visible cuts, burns, or other injuries on the body
- Unexplained bruises or wounds
- Wearing long sleeves or pants even in hot weather
- Carrying sharp objects or other items that could be used for self-harm
- Excessive preoccupation with pain or self-injury
- Changes in mood, behavior, or sleep patterns
- Withdrawal from social activities or relationships
- Expressions of self-hate or self-criticism
How can I help someone who is self-harming?
Express concern and support in a non-judgmental way. Encourage them to seek professional help from a therapist or other mental health professional. Avoid minimizing their pain or trying to solve their problems for them. Offer practical assistance by helping them create a safety plan or connect them with support resources.
Is self-mutilation a sign of mental illness?
Self-mutilation can occur in people with various mental health conditions, including depression, anxiety disorders, post-traumatic stress disorder, and borderline personality disorder. However, self-harm can also occur in individuals who do not have a formally diagnosed mental illness. It’s crucial to remember that self-harm behaviors are a symptom of underlying distress, and addressing the underlying causes is essential for recovery.
What is the best way to talk to someone about self-mutilation?
Approach the conversation with empathy and compassion. Start by expressing your concern and letting them know that you’re there to support them. Listen attentively to their experiences without judging or dismissing their feelings. Encourage them to seek professional help but avoid forcing or pressuring them.
Risk For Self Mutilation Nursing Care Plan
https://youtube.com/watch?v=qYL1wpdbLDI
Conclusion
Addressing self-harm is a complex challenge that requires a compassionate and multifaceted approach. By understanding the underlying causes, risk factors, and effective interventions, nurses can empower individuals at risk for self-mutilation to embark on a journey toward recovery. Through comprehensive nursing care plans, therapeutic support, and a commitment to building resilience, we can help break the cycle of self-harm and promote healing and well-being.
Are you interested in learning more about self-harm and how to support someone who might be struggling with this issue?






