It’s a joyous moment, bringing a new life into the world. But for new mothers who have undergone a Cesarean section, the path to recovery can be riddled with unexpected challenges. While the focus is often on the physical healing of the surgical incision, there’s a whole world of potential complications and emotional adjustments that need to be addressed. This is where the expertise of nurses comes in, armed with their knowledge of nursing diagnoses for postpartum Cesarean section, they can effectively provide individualized care and support.

Image: www.scribd.com
This article dives into the common nursing diagnoses encountered in the postpartum period following a Cesarean section, exploring the underlying factors, signs and symptoms, and importantly, the interventions nurses can implement to ensure a smooth recovery for mothers and their newborns.
Understanding Cesarean Section Recovery
A Cesarean section, also known as a C-section, is a surgical procedure where a baby is delivered through an incision made in the mother’s abdomen and uterus. While it’s a life-saving procedure in many cases, it comes with its own set of unique recovery challenges compared to vaginal deliveries.
Physical Challenges:
- Pain Management: Post-surgical pain is a significant concern. The incision site can be tender and sensitive, requiring effective pain management strategies.
- Wound Healing: The healing process for a C-section incision can take several weeks, and proper wound care is crucial to prevent infection.
- Limited Mobility: Mothers may experience restricted movement due to pain, discomfort, or safety precautions, limiting their ability to care for themselves and their newborns.
- Bowel Function: Constipation is a common side effect as anesthesia and medications can slow down the digestive system.
- Urinary Incontinence: Some mothers may experience temporary incontinence due to weakened pelvic floor muscles.
- Blood Clots: There is a risk of developing blood clots, especially in the legs, following surgery.
Emotional Challenges:
- Disappointment: Some mothers may feel disappointed if they were hoping for a vaginal birth and have to undergo a C-section.
- Anxiety: Postpartum anxiety can be amplified following a C-section, arising from the surgery itself, the recovery process, and adjusting to motherhood.
- Body Image Concerns: Mothers may experience feelings of insecurity about their bodies due to the surgical scar and potential changes in shape.
- Lack of Confidence: Limited mobility and potential complications can lead to feelings of inadequacy in caring for the newborn.
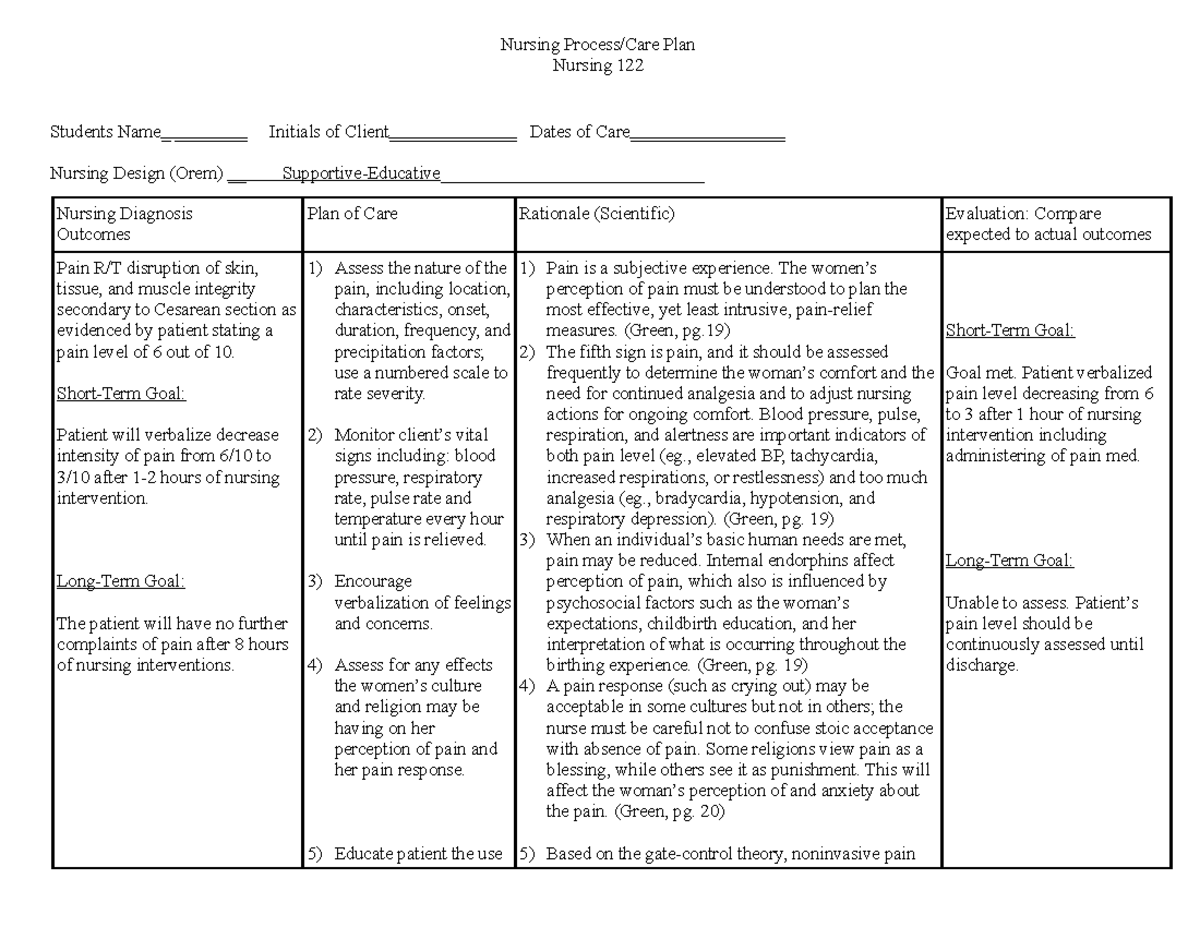
Image: www.studocu.com
Common Nursing Diagnoses for Postpartum Cesarean Section
Nurses play a crucial role in identifying and addressing potential problems during the postpartum period after a Cesarean section. Here are some of the most common nursing diagnoses they encounter:
1. Acute Pain
Pain is a top priority during the initial recovery period. The nursing diagnosis of “Acute Pain” focuses on the intensity, location, and quality of the pain experienced by the mother.
Interventions:
- Pain Medication: Regular administration of analgesics, such as IV pain medications, and transitioning to oral medication as tolerated.
- Positioning: Encouraging side-lying or using pillows for support to reduce pressure on the incision.
- Heat Therapy: Warm compresses can be applied to the incision area for pain relief.
- Non-Pharmacological Measures: Techniques like relaxation exercises, deep breathing, and guided imagery can also be helpful.
2. Risk for Infection
Infection is a significant concern after any surgical procedure. The nursing diagnosis of “Risk for Infection” focuses on identifying factors that increase the likelihood of infection, such as compromised skin integrity due to the incision.
Interventions:
- Wound Care: Maintaining a clean incision site, ensuring proper dressing changes and monitoring for signs of infection like redness, swelling, or drainage.
- Hand Hygiene: Emphasizing the importance of hand hygiene for both the mother and healthcare providers to minimize the risk of infection.
- Antibiotics: Administering prophylactic antibiotics to reduce the risk of infection.
3. Impaired Physical Mobility
Limited mobility is a common challenge after a C-section. The nursing diagnosis of “Impaired Physical Mobility” refers to the mother’s inability to move freely and comfortably due to pain, incision discomfort, or safety precautions.
Interventions:
- Ambulation: Gradually encouraging the mother to walk and move around as tolerated, starting with assisted ambulation and progressing to independent walking.
- Pain Management: Adequate pain management is essential to promote mobility.
- Positioning: Helping the mother get into comfortable positions to reduce strain on the incision site.
4. Constipation
Constipation is a frequent side effect after a C-section. The nursing diagnosis of “Constipation” addresses the delay or difficulty in bowel movements, primarily due to the effects of anesthesia, pain medication, and decreased mobility.
Interventions:
- Fluid Intake: Encouraging ample fluid intake to soften stools and promote bowel regularity.
- Fiber Intake: Recommending a high-fiber diet rich in fruits, vegetables, and whole grains to facilitate bowel movements.
- Laxatives: Using stool softeners or laxatives as prescribed by a healthcare provider.
5. Risk for Ineffective Breastfeeding
Even though having a Cesarean section doesn’t directly impede breastfeeding, it can create additional challenges. The nursing diagnosis of “Risk for Ineffective Breastfeeding” recognizes these associated hurdles.
Interventions:
- Skin-to-Skin Contact: Promoting early and frequent skin-to-skin contact between the mother and baby.
- Lactation Consultant: Connecting mothers with lactation consultants for personalized support and techniques.
- Positioning and Latch: Assisting mothers with finding comfortable breastfeeding positions and ensuring proper latch.
6. Anxiety
The physical and emotional demands of recovery after a Cesarean section can contribute to increased anxiety. The nursing diagnosis of “Anxiety” reflects the mother’s feelings of nervousness, apprehension, and heightened stress.
Interventions:
- Emotional Support: Providing empathetic listening and reassurance to help the mother cope with her anxiety.
- Education and Information: Sharing information about the recovery process, addressing concerns, and providing clear expectations.
- Stress Management Techniques: Teaching relaxation techniques, deep breathing exercises, and guided imagery to reduce anxiety.
- Support Groups: Encouraging mothers to connect with postpartum support groups to share experiences and find community.
7. Situational Low Self-Esteem
Postpartum changes in body image, limited mobility, and potential complications can impact a mother’s self-esteem. The nursing diagnosis of “Situational Low Self-Esteem” addresses these feelings of inadequacy, insecurity, and self-doubt.
Interventions:
- Positive Reinforcement: Acknowledging the mother’s strengths and accomplishments during her recovery.
- Body Image Support: Encouraging self-acceptance and providing resources for coping with body image concerns.
- Self-Care Practices: Promoting self-care activities that contribute to the mother’s well-being, such as taking time to relax, exercise, and engage in enjoyable activities.
8. Risk for Altered Family Processes
The recovery process after a Cesarean section can affect family dynamics and interactions. The nursing diagnosis of “Risk for Altered Family Processes” considers how changes in the mother’s role and responsibilities impact the family as a whole.
Interventions:
- Family Involvement: Encouraging family members to participate in the mother’s care and provide support.
- Communication: Facilitating open communication within the family to address concerns and build understanding.
- Support Systems: Connecting the family with community resources or support groups to help them navigate the postpartum period.
Nursing Diagnosis For Postpartum C Section
Conclusion: A Holistic Approach to Postpartum Cesarean Section Care
In the world of postpartum care, understanding the specific nursing diagnoses for Cesarean section recovery is crucial. Nurses play a vital role in identifying potential challenges and implementing targeted interventions to ensure the well-being of mothers and their newborns. From pain management and wound care to addressing emotional adjustments and family dynamics, nurses provide individualized care tailored to meet each mother’s unique needs. By taking a holistic approach that considers both physical and emotional aspects of recovery, nurses empower mothers to regain strength, build confidence, and enjoy the joys of motherhood with their new little one.
Whether you’re a new mother navigating the challenges of postpartum recovery or a healthcare professional seeking to deepen your understanding of this area, this article serves as a valuable resource. As always, remember that seeking personalized advice from healthcare providers is essential for individual care plans.






