Imagine the journey of bringing a new life into the world, a moment of unbridled joy and anticipation. Yet, for some expectant mothers, this journey is complicated by gestational diabetes mellitus (GDM), a condition that develops during pregnancy. The diagnosis can be unsettling, but understanding the nuances of gestational diabetes and the role of nursing care can empower expectant mothers and their families to navigate this challenge with informed confidence.
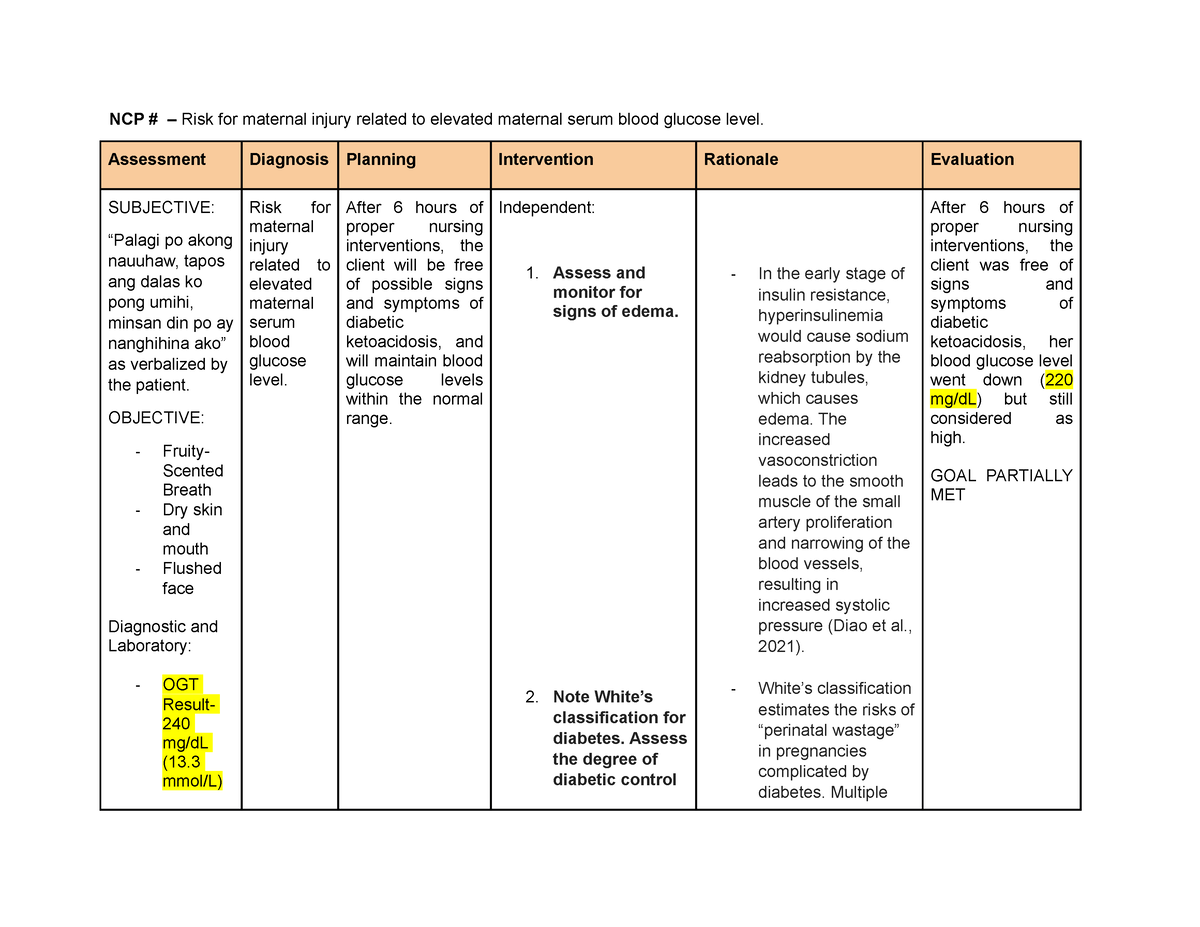
Image: www.myxxgirl.com
This nursing care plan delves into the intricacies of gestational diabetes, emphasizing evidence-based interventions and crucial nursing roles. We will explore the causes, risks, and management strategies that contribute to a safe and healthy pregnancy for both mother and baby.
Understanding Gestational Diabetes: The Basics
Gestational diabetes mellitus (GDM) is a condition where a woman develops high blood sugar levels for the first time during pregnancy. While usually temporary, GDM poses potential risks for both mother and baby. The primary cause of GDM is a complex interplay of hormonal changes, particularly insulin resistance, experienced during pregnancy. Insulin, a hormone produced by the pancreas, plays a crucial role in regulating blood sugar levels. During pregnancy, placental hormones like human placental lactogen (hPL) interfere with the action of insulin, leading to elevated blood sugar levels.
The impact of GDM can be far-reaching. If left unmanaged, GDM increases the risk of:
- Preeclampsia: A serious pregnancy complication marked by high blood pressure and protein in the urine.
- Premature birth: Delivery earlier than 37 weeks gestation, increasing the risk of complications for the newborn.
- Macrosomia: A baby born larger than average, associated with birth injuries and complications.
- Stillbirth: A tragic loss of a baby after 20 weeks gestation.
- Increased risk of developing type 2 diabetes later in life for both the mother and child.
The Essential Role of Nursing Care
The nursing care plan for gestational diabetes is a vital component of safe motherhood. Nurses play a pivotal role in educating expectant mothers, monitoring their condition, and providing support through personalized interventions. Here, we will explore the key elements of this comprehensive care plan:
1. Assessment and Diagnosis: Unveiling the Underlying Factors
The journey for GDM management begins with a thorough assessment. Nurses, acting as the eyes and ears of the healthcare team, work collaboratively with physicians to gather critical information about the pregnant woman’s health history, current symptoms, and risk factors. This information helps in making a timely and accurate diagnosis.
The diagnosis often begins with a glucose challenge test (GCT), a screening test where patients drink a sugary beverage and have their blood sugar levels checked after a specified period. If the GCT is abnormal, an oral glucose tolerance test (OGTT) is performed, a more comprehensive diagnostic test.

Image: www.scribd.com
2. Blood Sugar Monitoring: Keeping a Close Eye on Blood Glucose Levels
Blood sugar monitoring is a fundamental aspect of managing GDM. Nurses guide pregnant women in understanding the importance of regular monitoring, teaching them how to use a home blood glucose meter effectively. This empowers women to take control of their health and stay informed about their blood sugar fluctuations.
Frequency of monitoring depends on the individual’s blood sugar levels and overall health status. Some women may require monitoring several times a day, while others may need less frequent checks.
3. Lifestyle Modifications: Embracing a Healthier Path
Lifestyle modifications are often the cornerstone of managing gestational diabetes. Nurses collaborate with registered dietitians to create personalized meal plans that are balanced, nutrient-rich, and tailored to the individual’s preferences and needs. The focus is on making gradual changes to eating habits rather than drastic overhauls:
- Balanced Diet: This involves incorporating whole grains, fruits, vegetables, lean proteins, and low-fat dairy products, while limiting sugary drinks, refined grains, and processed foods.
- Regular Physical Activity: Engaging in moderate-intensity exercise for at least 30 minutes most days of the week can help improve insulin sensitivity and better manage blood sugar levels. Walking, swimming, and low-impact aerobics are excellent options.
- Stress Management: Stress can significantly impact blood sugar control. Nurses encourage pregnant women to adopt stress-reducing techniques like yoga, meditation, or spending time in nature.
4. Medication: When Lifestyle Changes Aren’t Enough
In some cases, lifestyle modifications alone may not be enough to achieve optimal blood sugar control. Nurses are essential partners in helping pregnant women understand the role and potential benefits of medication. Insulin therapy is commonly used to effectively regulate blood sugar levels in GDM.
Nurses provide ongoing support and education about the different types of insulin, administration techniques, and potential side effects. Patient education is crucial in promoting compliance and ensuring medication safety.
5. Antepartum Monitoring: Ensuring a Healthy Pregnancy
Regular antenatal care visits are crucial in monitoring the progress of the pregnancy and the woman’s overall health. Nurses play an active role in monitoring fetal growth, checking the blood sugar levels of both mother and baby, monitoring blood pressure, and addressing any concerns that may arise.
During these visits, nurses provide ongoing education on blood sugar management and answer any questions or concerns the patient may have. This constant communication fosters a trusting relationship and ensures the pregnant woman feels empowered and supported.
Navigating Labor and Delivery: A Teamwork Approach
The management of GDM extends to labor and delivery. Nurses are key players in ensuring a safe and healthy birthing experience for both mother and baby. Close monitoring of blood sugar levels during labor is essential, and insulin therapy may be adjusted as needed.
For mothers with GDM, cesarean deliveries are often recommended, especially for babies with macrosomia. However, the decision is ultimately made on a case-by-case basis by the healthcare team, considering the individual mother’s health and the baby’s well-being.
The Postpartum Period: A Time for Continued Support
After delivery, the nursing care plan remains crucial. Nurses continue to monitor blood sugar levels, provide guidance on breastfeeding and nutrition, and facilitate follow-up appointments with healthcare providers.
The postpartum period is a time when women can discuss their experiences with GDM, express concerns and receive support in transitioning to life with a newborn. Nurses work collaboratively with other healthcare professionals to ensure the mother and baby are both healthy and thriving.
Nursing Care Plan For Gestational Diabetes Mellitus
Conclusion: Empowering Women to Thrive
The nursing care plan for gestational diabetes is a beacon of hope and empowerment for women with GDM, offering a comprehensive approach to ensure their safety and the well-being of their babies. From the initial diagnosis to postpartum care, nurses play a vital role in educating, monitoring, and supporting pregnant women throughout their journey.
By embracing empowered self-management, seeking professional guidance and support, and adopting healthier lifestyle choices, expectant mothers with GDM can navigate pregnancy with confidence, contributing to a future filled with joy and healthy growth for both themselves and their little ones.






